Introduction of Thrombus and Postmortem Clot
Thrombus and Postmortem Clot are two different blood clot formations with unique causes and implications.
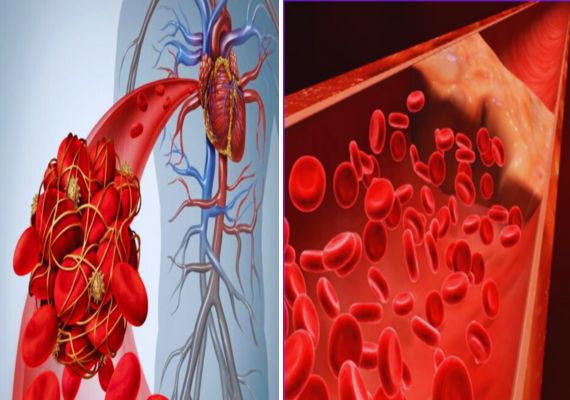
A thrombus is a blood clot that forms within living people’s blood vessels due to injury, inflammation, or medical conditions that obstruct blood flow; this may lead to serious health complications including heart attacks or strokes. Artery thrombi and venous thrombi are the two types of thrombi most likely affected.
Postmortem or “cadaveric” clots form after death as the result of blood settling and coagulating due to gravity in various body parts, making their identification vital in forensic science for estimating the time of death estimates and differentiating them from clots formed during life.
Proper differentiation of postmortem from life clots requires looking at factors like clinical history, gross appearance, microscopic features, and sometimes further testing, accurate medical diagnosis, as well as effective investigations, which require this distinction between types.
what is Thrombus?
A thrombus is an abnormal blood clot that forms within the circulatory system, typically within blood vessels or the heart. It often results from factors that disturb the normal flow, leading to accumulations of platelets, fibrin, and other cell components, thrombi may also be the result of medical conditions or injuries that present themselves as causes. They pose severe health risks.
Thrombus formation can take place both in arteries and veins, creating arterial thrombi and venous thrombi, respectively. Artery thrombi are composed of platelets and fibrin; these typically form in areas affected by atherosclerosis or plaque buildup and can block blood flow to critical organs, leading to serious medical consequences like heart attacks or strokes.
Venous thrombi are composed of fibrin and red blood cells and tend to form in veins in the legs, especially deep veins known as deep vein thrombosis (DVT). If they dislodge and travel through the bloodstream, if dislodged they could lead to pulmonary embolism by blocking off oxygen-rich blood flow to the lungs.
Thrombus formation can be caused by various risk factors, including genetics, age, lifestyle, and certain medical conditions like hypertension, diabetes, or clotting disorders. Treatment and prevention strategies often include anticoagulant medication.
Similarly, lifestyle modifications with surgical interventions are the last resort if complications develop quickly. Recognizing and treating thrombi as soon as they arise is vital in order to avoid serious health consequences and preserve wellness.
Causes of thrombus
Here are some of the primary causes of thrombus formation:
- Endothelial Injury: Damage to the inner lining of blood vessels, known as endothelium, is known to trigger thrombus formation. Such damage may be due to trauma, surgery, or inflammation – all factors which could potentially increase risk.
- Stasis of Blood Flow: When blood flow decreases or becomes stagnant, it can increase the risk of thrombus formation. This often occurs as a result of immobility or bed rest, or from veins with malfunctioning valves leading to venous thrombosis.
- Hypercoagulability: Certain medical conditions and genetic predispositions can increase the tendency of blood to clot. For instance, inherited thrombophilias (genetic predisposition to blood clotting) as well as acquired conditions like cancer, pregnancy or use of oral contraceptives can contribute to hypercoagulability.
- Atherosclerosis: Accumulated fatty plaques within an artery’s walls can damage endothelium cells and contribute to thrombus formation, potentially leading to arterial thrombosis and potentially leading to conditions such as heart attacks and strokes.
- Atrial Fibrillation: Uneven heart rhythms such as atrial fibrillation can disrupt normal blood flow within the atria and increase risk for thrombus formation that could potentially embolize and travel throughout your body.
- Inflammatory Conditions: Vasculitis is an inflammatory disorder that increases endothelial damage, increasing its chances of thrombus formation and leading to further endothelial damage and risk.
- Smoking: Nicotine damage damages blood vessel walls and contributes to atherosclerosis, increasing the chances of thrombus formation.
- Obesity: Excess body weight can exacerbate inflammation and increase the risk of thrombosis.
- Medication: Hormone replacement therapy and certain chemotherapy drugs may increase your risk of blood clot formation.
what is Postmortem Clot?
Postmortem or “cadaveric clot,” as it’s also known, is an unusual form of blood clot that develops after death has taken place and in its circulatory system. These postmortem clots form naturally as part of postmortem changes taking place within bodies after death unlike living individuals’ thrombi, which form pathologically due to pathologies, postmortem clots form due to gravity and cessation of circulation at death.
As soon as someone passes, their heart stops pumping blood, leading to its concentration in various parts of their body most commonly in their lower extremities. Oxygen evaporates from this pooled blood pooling process, coagulation occurs and postmortem clots form within veins or even heart chambers often having gel-like consistency and often occurring after death.
Postmortem clots play an essential part in forensic science and determining the time of death, providing pathologists and investigators with valuable insights. Differentiating them from thrombi formed during life is key for accurate estimations of the time of death estimates as well as understanding postmortem changes to bodies after death.
Studying postmortem clots also plays a vital part of forensic medicine aiding investigations of unexplained deaths or criminal cases.
Causes of Postmortem Clot
Here are the main causes of postmortem clot formation:
- Cessation of Blood Circulation: One of the primary factors contributing to postmortem clot formation is when blood circulation ceases altogether, typically following cardiac death when no longer flows through vascular channels as it did prior to death.
- Gravity: Gravity plays a crucial role in postmortem clot formation. Blood, which contains clotting factors, tends to pool and accumulate in certain parts of the body – typically the lower extremities – due to gravitational forces.
- Loss of Oxygenation: Once the blood stops flowing and oxygen exchange ceases, its concentration in affected areas begins to decrease and oxygen can leave their bodies. This alteration in oxygen status may trigger the coagulation cascade and lead to clot formation.
- Coagulation Factors: Blood contains various coagulation factors which promote clot formation. Without anticoagulant mechanisms in place, these factors contribute to postmortem clot formation.
- Temperature: The process of cooling the body after death (algor mortis) can have an impactful influence on the coagulation process. Lower temperatures can reduce enzyme reactions and delay clot formation.
- Postmortem Interval (PMI): The postmortem interval (PMI) refers to the time elapsed since death has taken place and can have an impactful impact on both its extent and characteristics of postmortem clot formation, possibly continuing during this interval period. Clotting may continue developing even while you wait!
- Environmental Aspects: Environment-related variables such as ambient temperature and humidity can have an effect on postmortem clot formation rates and appearance.
- Position of the Body: The position of a deceased at death and after is a key factor when it comes to postmortem clot formation. For instance, lying flat upon their backs may lead to more clots forming nearer their lower extremities than elsewhere on their body.
- Underlying Medical Conditions: Certain underlying medical conditions, such as coagulation disorders, can impact how blood clots after death.
The key difference between Thrombus and Postmortem Clot
Here’s a comparison chart summarizing the key differences between Thrombus and Postmortem Clot:
| Characteristic | Thrombus | Postmortem Clot |
|---|---|---|
| Formation | Forms in living individuals due to pathological factors such as injury, inflammation, or underlying medical conditions | Develops naturally in a deceased individual after death has occurred due to gravity and cessation of circulation |
| Composition | Composed of platelets, fibrin, and cellular components | Composed primarily of fibrin and red blood cells |
| Location | Arterial thrombi can form in arteries; venous thrombi develop in veins | Typically found in veins, especially deep veins of the lower extremities |
| Health Implications | Can obstruct blood flow and lead to serious health issues such as heart attacks or strokes | No direct health implications as it forms postmortem; plays a role in forensic science |
| Causes | Underlying medical conditions, injuries, or risk factors contribute to thrombus formation | Formation is a natural consequence of postmortem changes in a deceased body |
| Differentiation | Diagnosed based on clinical history, imaging, microscopic examination, and laboratory tests | Distinguished from antemortem clots through forensic examination, location, and pattern |
| Clinical Relevance | Significant for diagnosis and treatment of thrombotic conditions in living individuals | Critical in forensic medicine for estimating the time of death and understanding postmortem changes |
| Management | Managed with anticoagulant medications, lifestyle changes, and surgical interventions | No medical management required; studied for forensic purposes |
How are Thrombi and Postmortem Clots Formed?
Formation of Thrombi:
- Endothelial Injury: Thrombi typically form due to endothelial damage. When the inner lining of blood vessels (endothelium) is compromised, blood components that promote clotting become exposed. Common sources of endothelial injury include plaque buildup in arteries (atherosclerosis), trauma or inflammation as potential culprits for damage.
- Stasis of Blood Flow: Reduced or stagnant blood flow is known as stasis, and can contribute to thrombus formation. When blood slows or becomes stagnant, clotting factors accumulate and initiate the coagulation cascade, creating the perfect conditions for stasis-induced thrombi to form. Prolonged immobility or conditions like deep vein thrombosis (DVT) can also result in stasis-induced thrombi formation.
- Hypercoagulability: Certain medical conditions, genetic factors, and medications can increase the blood’s tendency to clot, leading to hypercoagulability. Conditions like thrombophilias (genetic predisposition to clotting) and cancer may contribute to this tendency and lead to the formation of thrombi.
- Blood Constituents: Thrombi are comprised of platelets, fibrin, and other blood components that interact to initiate clotting processes by attaching themselves to damaged vessel walls; platelets then aid the process by adhering themselves directly to damaged artery walls, while fibrin acts as an adhesive mesh which traps blood cells within it, ultimately creating a clot that can stop bleeding.
Formation of Postmortem Clots:
- Stoppage of Blood Circulation: Following death, postmortem clots often form when the heart ceases beating, stopping blood circulation altogether and stopping its movement through the circulatory system. Without a heartbeat force to push blood through circulation channels, blood cannot move freely throughout circulation systems like circulatory systems.
- Gravity: Gravity plays an integral part in postmortem clot formation. Once dead, blood tends to collect in dependent parts of the body–primarily the lower extremities–due to gravitational effects.
- Loss of Oxygenation: Once the blood stops moving and oxygen exchange stops, oxygen depletes from dependent areas’ blood. This change in oxygenation status may trigger the coagulation cascade and result in clot formation.
- Coagulation Factors: Blood contains various coagulation factors that help facilitate blood clotting. When combined with nonfunctioning anticoagulant mechanisms and these coagulation factors, postmortem clot formation can occur due to postcoagulation coagulation processes.
- Temperature: The process of cooling after death (algor mortis) can have an impact on coagulation. Lower temperatures can inhibit enzyme-based reactions and delay clot formation.
Where do Thrombi and Postmortem Clots Typically Occur in the Body?
Due to their unique formation processes, thrombi and postmortem clots tend to manifest themselves differently throughout the body. Thrombi, pathological blood clots that develop during life, typically affect arteries or veins depending on their type.
Arterial thrombi can form in critical arteries such as those located within the heart or brain (coronary or cerebral) which could lead to heart attacks or strokes; on the other hand, venous thrombi typically form in veins, particularly deep veins in legs resulting in deep vein thrombosis (DVT).
Postmortem clots (also referred to as cadaveric clots) are formed through natural postmortem processes in deceased individuals and typically form in dependent areas under gravity’s influence after death, typically near dependent veins such as those located in the lower extremities, such as popliteal, femoral and saphenous veins.
They may also form in heart chambers like the right atrium if early postmortem processes did not fully evacuate all chambers of the heart during the early postmortem period, their exact formation depends upon where the body lies after death as gravity plays an essential part in their formation.
How Do Thrombi and Postmortem Clots Look Different
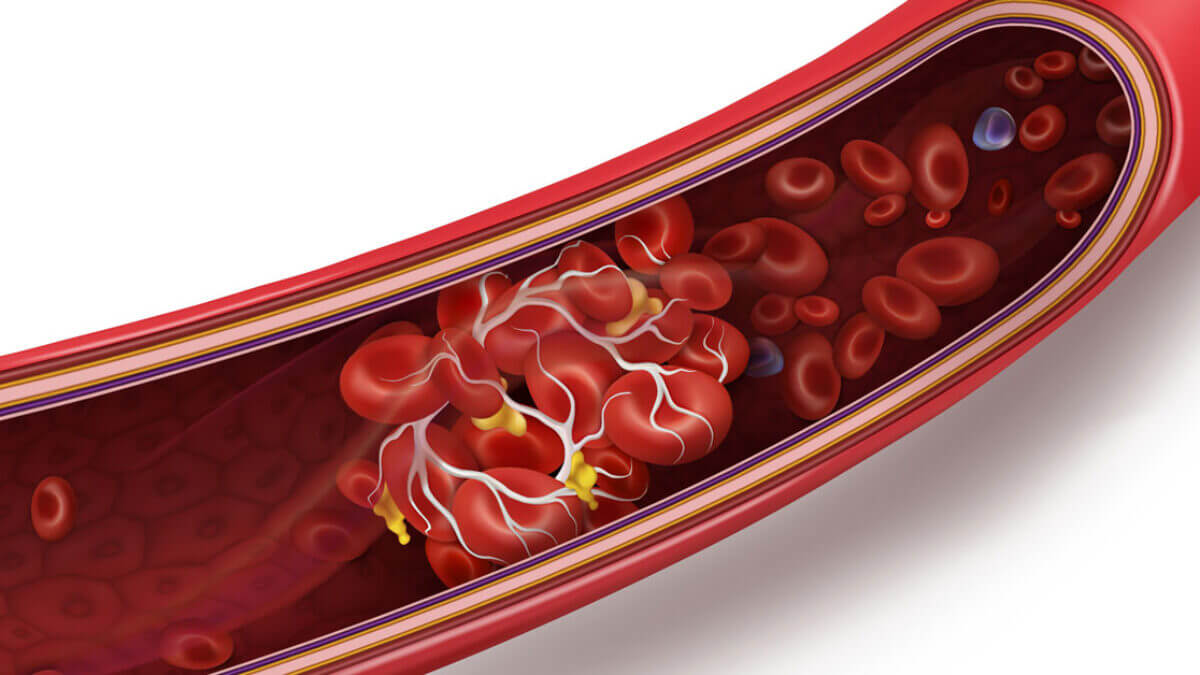
Living individuals often exhibit certain distinctive features when it comes to thrombi. They typically appear as gel-like masses within blood vessels and can vary in size and color, depending on their location and composition; arterial thrombi tend to be paler due to high concentrations of platelets and fibrin while venous ones might look darker due to higher concentrations of red blood cells and fibrin.
Thrombi can partially or fully block blood vessels, potentially leading to tissue damage or downstream complications; on imaging studies thrombi can often be visualized filling holes within vessel lumens, signifying blockages within vessel lumens indicating obstruction within vessel lumens indicating blockages within vessel lumens indicating blockage within vessels lumens indicating potential blockages within vessel lumens that indicate such obstruction.
Postmortem clots exhibit their own distinct features. Usually appearing dark red to maroon in color with a gelatinous consistency, postmortem clots often form in areas influenced by gravity such as lower extremities or right atrium of the heart. Their presence here and gravity-dependent nature are indicators of postmortem changes, unlike thrombi.
Postmortem clots do not correlate directly with any damage; instead, they result from cessation of circulation after death and pooling blood into dependent areas that accumulates until death finally occurs and pools blood pools at rest in such dependent areas resulting in pooled blood pools of dependent areas due to cessation of circulation upon death leading to pooling of blood pooling as resultant pools clots.
Diagnostic System
Diagnostic System for Thrombi
Clinical History and Symptoms: Physicians often begin their diagnosis process by conducting a comprehensive medical history review and assessing symptoms that may include chest pain, shortness of breath or leg swelling depending on where thrombus formation has taken place.
Physical Examination: A physical exam may reveal signs associated with thrombosis, including swelling, redness and tenderness in the affected area.
Imaging techniques may aid in diagnosing thrombi, including:
- Ultrasound: Used to visualize blood flow and detect deep vein thrombosis (DVT). Computed Tomography (CT).
- Magnetic Resonance Imaging (MRI): These imaging methods are capable of detecting various thrombi throughout the body, such as pulmonary emboli in lungs or cerebral thrombosis in brain.
- Angiography: Invasive procedures like angiography can directly visualize blood vessels and detect thrombi.
Laboratory Tests: Blood tests such as D-dimer levels or coagulation profiles provide useful additional information in diagnosing thrombi.
Diagnostic System for Postmortem Clots:
- Forensic Examining: Postmortem clots often surface during postmortem forensic exams of deceased individuals, with experts conducting an in-depth assessment that evaluates both their condition and any specific clots present or observed during their review of postmortem bodies.
- Location and Pattern: Forensic professionals pay particular attention to the location and pattern of postmortem clots as these tend to form in dependent areas due to gravity. Clumps seen on the lower extremities or right atrium of the heart indicate normal postmortem changes.
- Differentiation: Distinguishing between postmortem clots and those formed during life is vital, with factors like postmortem interval (time since death), absence of vital signs, and gravitational force playing an integral part.
- Ancillary Testing: Additional tests or imaging may be conducted to establish the postmortem nature of blood clots in complex forensic investigations.
Treatment Option
Treatment Options for Thrombi
- Anticoagulant Medications: Heparin and warfarin are commonly prescribed medications used to prevent the expansion of existing thrombi and prevent new ones from forming, as they interfere with clotting processes and the clotting cycle.
- Thrombolytic Therapy: When severe thrombosis strikes, particularly cases like massive pulmonary embolism or acute myocardial infarction (heart attack), tissue plasminogen activators (TPAs) may be administered as an expedient means of breaking up the clot quickly and dissolving it more rapidly.
- Antiplatelet Medication: Antiplatelet medications such as aspirin and clopidogrel may help to inhibit platelet aggregation and lower the risk of arterial thrombosis.
- Compression Stockings: Wearing compression stockings may help protect against deep vein thrombosis (DVT) by helping prevent further clot expansion and alleviating symptoms like leg swelling.
- Surgical Interventions: When thrombi are causing severe blockages or complications, surgical procedures like thrombectomy (the removal of the clot through surgical means) or angioplasty with stent placement may be required to restore normal flow and remove complications caused by blockages or obstruction.
- Lifestyle Modifications: Engaging in healthier behaviors such as maintaining a healthy weight, regular physical activity, and quitting smoking may reduce the risk of thrombosis in those with risk factors.
Treatment Options for Postmortem Clots:
Postmortem Clots (or Cadaveric Clots) do not need medical intervention as they form after death and do not pose direct health concerns, They can be helpful when investigating postmortem changes as part of forensic medicine studies to ascertain the timing of death and assess postmortem changes, thus experts often take postmortem clots into consideration as part of their investigations.
What are Thrombus and Postmortem Clot risk factors?
Thrombus Risk Factors
Thrombosis, also known as blood clots, can form within living individuals and lead to serious health consequences.
Common risk factors associated with the formation of thrombi include
- Endothelial Injury: Conditions or factors that damage the inner lining of blood vessels (endothelium) can increase your risk of thrombus formation, including atherosclerosis, trauma, and inflammation. Examples include atherosclerosis, trauma, and inflammation.
- Stasis of Blood Flow: Reduced or stagnant blood flow increases the likelihood of thrombus formation, and can be caused by prolonged inactivity, bed rest or conditions affecting venous return such as varicose veins. Risk factors may include long periods of inactivity such as prolonged immobility or bed rest as well as conditions that prevent proper vein return like varicose veins.
- Hypercoagulability: Conditions that increase the tendency for blood to clot, such as genetic factors or acquired conditions, are serious risk factors. Examples include inherited thrombophilias, cancer treatments, pregnancy and certain medications.
- Atrial Fibrillation: Abnormal heart rhythms like atrial fibrillation may restrict blood flow within the heart, potentially leading to atrial thrombi that could embolize other parts of your body and threaten life.
- Age: Aging increases one’s risk for thrombosis.
- Obesity: Obesity has been linked with inflammation and an increased risk of thrombus formation.
- Smoking: Cigarette smoking damages blood vessel walls and increases your risk of atherosclerosis and thrombosis.
- Medical Conditions: Diabetes, hypertension, and clotting disorders can increase the risk of thrombus formation.
- Surgery and Trauma: Substantial surgery or trauma may damage blood vessels, leading to thrombosis.
Postmortem Clot (Cadaveric Clot) Risk Factors
Postmortem clots are naturally occurring and do not have traditional risk factors associated with them like thrombi do. Instead, they form as part of postmortem changes after death in deceased bodies, with their presence and characteristics determined by factors like time since death, body position and environmental conditions.
They do not correlate to any specific medical conditions or lifestyle choices like thrombi do.
Summary
A thrombus is a blood clot formed due to pathological processes in living individuals that can result in serious health concerns. Composed of platelets, fibrin, and cell components, thrombus requires medical supervision for its management and can have devastating health implications.
Postmortem clots also referred to as cadaveric clots, develop naturally in deceased individuals after death due to gravity and circulation disruptions, usually as soon as gravity sets in.
Comprised mostly of fibrin and red blood cells, postmortem clots play an essential role in forensic medicine as they help estimate the time of death and understand postmortem changes. Their differentiation from thrombus is key for accurate diagnoses and investigations.